I am a Band 7 midwife with a shift management role at Tameside General Hospital, and I used my Iolanthe Midwives Award to fund taking a Midwifery Critical Care module at Masters Level.
 Our maternity unit is a smaller one, so we don’t have facilities for intermediate care. This means that postnatal women who also have serious health complexities are best cared for over on the hospital’s general high dependency unit (HDU), where, sadly, their babies cannot room in with them.
Our maternity unit is a smaller one, so we don’t have facilities for intermediate care. This means that postnatal women who also have serious health complexities are best cared for over on the hospital’s general high dependency unit (HDU), where, sadly, their babies cannot room in with them.
During the pandemic, the HDU beds were often full, meaning there was no space for our women to go there, and it became really clear for our staff that we wanted increased skills to give them optimal care. At the same time, the women themselves actually expressed appreciation that they got to stay in the maternity unit, since they could keep their babies with them, and they also benefited from continuity of carer, as they were often looked after by the same midwives over their stay.
I actually really like giving complex care; I have personal experience of a stay on an HDU, and I can bring that to the care I give.
I could see how much it worsened an already difficult time, to be separated from your baby, and I just felt I had to do something about it, so accessing this module was my first step.
Due to covid, the course was almost all distance learning, and that was tough. I missed the opportunity for practical sessions, but the networking opportunities were excellent, it was so helpful to hear what was being set up in other units far afield from us, and make just the right connections to help our plans.
There were staff from some excellent enhanced care units attending, and I was able to reflect on what we could learn from these – my presentation at the end was how about I was going to take forward what I learnt.
It was a challenge doing a fulltime course while also working fulltime during a pandemic – to say the least! - but it has absolutely been worth it. A key example is that previously, we didn’t accept anyone on our unit who needed an arterial line in place, as these lines need specialised care. But this was a skill we could learn; so we have now trained many of our staff in this.
Further, we have a new arrangement that if we don’t have a midwife with arterial line training on shift, we can ask for support from the theatre nurses who will attend to give this care, so these women can stay with us alongside their babies.
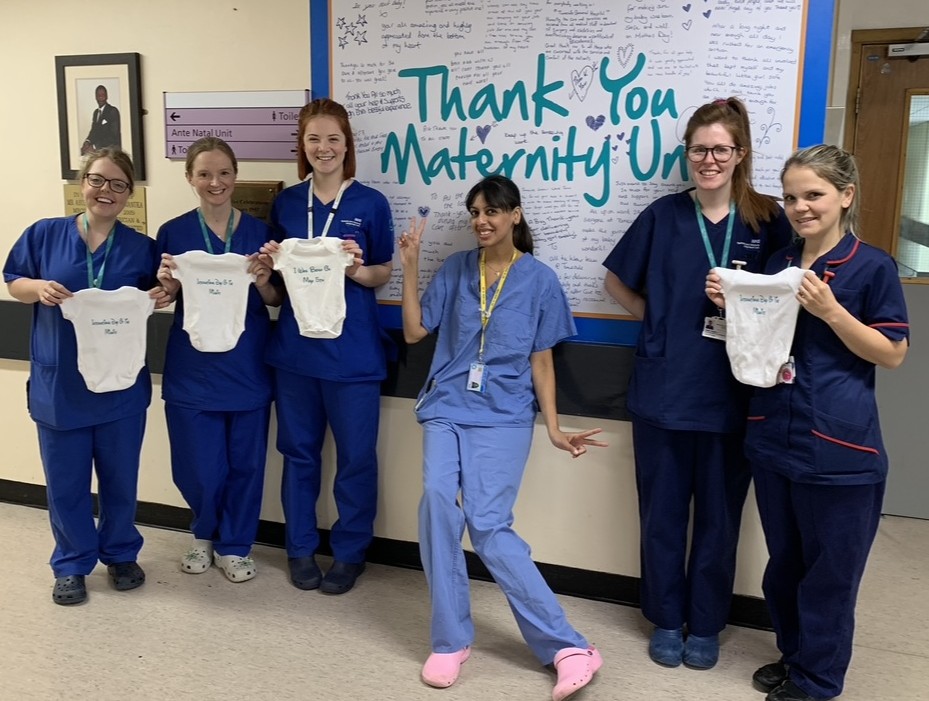
We are also keeping many women who have had serious haemorrhages, instead of transferring them, as we can now offer the level of care they need in situ.
We have introduced a critical care chart; and are promoting the core competencies for Labour Ward staff as recommended by the Royal College of Anaesthetists. And, although the Trust wasn’t able to fund me originally, they are now willing to prioritise sending more of our midwives on the Critical Care module. Personally, I have decided to continue with working towards an MSc, so later this year I will complete the Spontaneous Labour and Birth module, with the aim of protecting this as much as possible amid complex care.

It was my friend Nicolette Peel who told me about the Iolanthe Awards; I might never have taken this journey without her encouragement.
Nicolette died last year, and starting 2024, the Iolanthe Trust is offering a new Award to commemorate her life and her contribution to midwifery.
I would pass on Nicolette’s message to all those caring for birthing families – if you have a vision for care, then go for it